Introduction: Peripheral perfusion limitation is a potential biomarker of the severity and progression of sickle cell disease (SCD). Currently, there exists no direct means of quantifying perfusion deficits in SCD patients. Transcranial doppler ultrasonography offers a surrogate measure of perfusion and is highly operator dependent. Routine clinical screening of perfusion abnormalities with alternative modalities (e.g., positron emission tomography and magnetic resonance imaging) is challenging given high cost, requirement for sedation in young children, and need for trained personnel. The Combined Heat-Flux Temperature Sensor (CHFT+) is a novel noninvasive bio-heat perfusion sensor that measures peripheral perfusion in real time at depths of up to 1 cm by applying a minimal amount of heat to the skin surface. Because perfusion limitation is a hallmark of SCD, an improved understanding of its pathophysiology could potentially empower both patients and their physicians. The aim of this study was to evaluate the ability of the CHFT+ to detect differences in peripheral perfusion between healthy volunteers and patients with SCD.
Materials and Methods: The present study is an ongoing, non-randomized pilot study that aims to test the CHFT+ sensor's ability to detect impaired perfusion is pediatric SCD patients. We are actively enrolling pediatric patients (age 3-17) with SCD and healthy volunteers from 2 pediatric clinics to test the sensor. Peripheral perfusion measurements were obtained at 5 locations on the body (e.g., forehead, forearms, palms). All measurements were normalized against forehead perfusion values to account for individual variations. An independent-samples t-test was conducted to compare average rates of perfusion in patients with SCD and in healthy volunteers. The goal enrollment for this study is 52 patients (26 with SCD, 26 healthy controls) to detect a two-fold difference in perfusion with a power of 0.80.
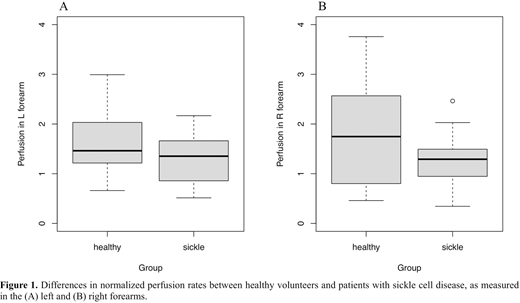
Interim Results and Discussion: To date, 31 participants have been enrolled, 10 (32%) of whom were patients with SCD. Overall, average perfusion rates were lower in the SCD group when compared to the healthy group, although these differences were not statistically significant. Representative measurements of perfusion in the right and left forearms, normalized against forehead rates, are shown in Figure 1. Normalized left forearm perfusion in healthy controls vs. SCD patients: avg = 1.77, SD = 0.95 vs. avg = 1.28, SD = 0.52, respectively [t(27) = 1.80, p = 0.08]; see Fig. 1a. Normalized right forearm perfusion in healthy controls vs. SCD patients: avg = 1.80, SD = 1.01 vs. avg = 1.31, SD = 0.60, respectively [t(25) = 1.55, p = 0.13]); see Fig. 1b.
Conclusions:At this time, our data suggest that the novel CHFT+ sensor is capable of detecting a modest difference in peripheral perfusion in children with SCD versus healthy controls, but this difference is not statistically significant due to limited enrollment. Additional enrollment will further define the utility of the CHFT+ sensor in this clinical population. Future studies should evaluate the sensor's capability to detect perfusion deficits in the adult SCD population, as well as measure perfusion variations that occur during SCD vaso-occlusive crises.
Diller:FluxTeq:Other: Partner.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal